cure for type 2 diabetes
Metabolic surgery
Metabolic surgery is one that allows the cure of diabetes and prevents its complications. It is performed in non-obese patients with a body mass index between 23 and 34 kg/m2 and associated metabolic syndrome.
It has been shown that performing this procedure reduces the need for medications in these patients almost 100% and achieves remission of the disease in more than 90% of type 2 diabetics (diabetes that is acquired in adulthood not associated with obesity).
The best results are observed with patients with less than 8 years of diabetes history.
The objective of surgical treatment is to improve the quality of life of patients, reaching normal blood glucose values without complementary medication, thus resolving diabetes and avoiding the complications it causes, increasing life expectancy with QUALITY.
Who are candidates for metabolic surgery?
- Patients with less than 10 years of diagnosis with type 2 diabetes
- Glycosylated hemoglobin greater than 7.5%.
- IMC: 23 – 34.
- Age: 18 – 65 years.
- Stable treatment for at least 6 months.
- C Peptide levels between 1 – 4.5.
Who is not a candidate for metabolic surgery?
- Patients with type 2 diabetes who already have complications: diabetic retinopathy, neuropathy or microangiopathy.
- Patients on hemodialysis or peritoneal dialysis.
- Insulin levels in the blood are very below normal or absent.
- Mental disorders (that do not allow following medical instructions)
- Pregnant patients.
- History of an operation on the stomach or small intestine (relative).
Glycemic control (independent of weight loss) is based on:
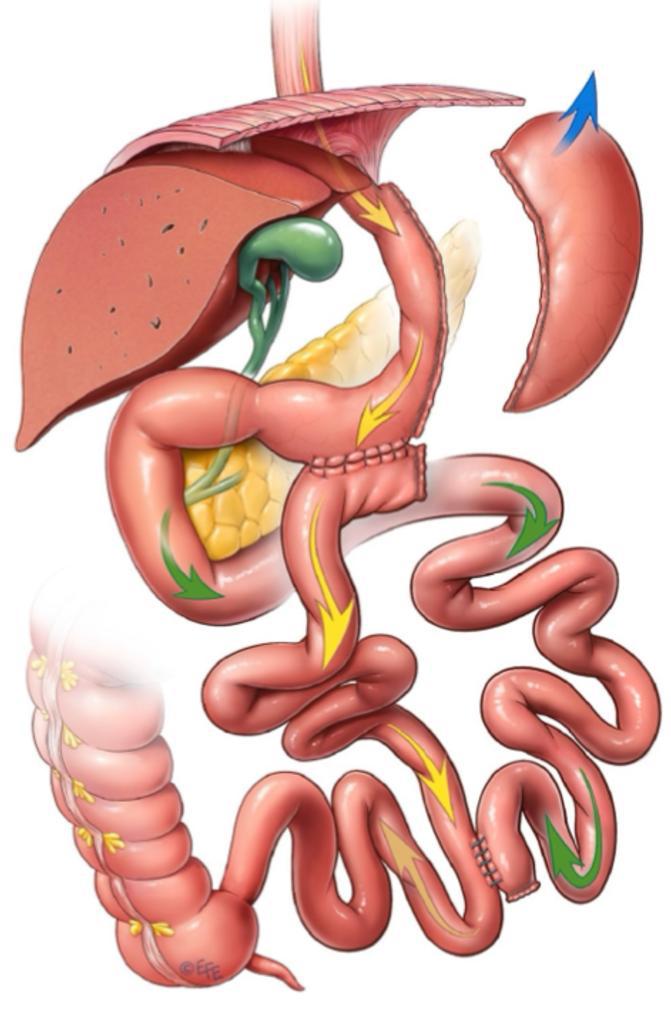
The foregut theory (exclusion of intestinal transit).- Inhibits the secretion of hormones related to insulin resistance, promotes incretins and cancels anti-incretins, potentiates insulin.
Another mediator with effects is GLP-1 (glucagon – like peptide – 1), a peptide that is produced in the distal intestine (distal intestine theory) in response to a mixed meal, it inhibits glycogenolysis, inhibiting glucagon, and prolongs gastric emptying. and intestinal motility; It is the most powerful incretin, promoting insulin secretion, and it also potentiates B cells with proliferative and anti-apoptoic activity, thus improving insulin sensitivity.
Peptide YY3 – 36 (PYY) decreases appetite. It is produced in the enteroendocrine cells of the ileum and colon, with a similar function to Ghrelin (appetite-regulating hormone).
In summary, avoiding the passage of food through the duodenum and reaching the end of the small intestine in less time causes an increase in insulin production, decreases the resistance of insulin receptors and absorbs less food.
With surgical procedures, percentages of diabetes resolution have been described as follows: 83 – 92% for gastric bypass and 95 to 100% for duodenal-jejunal bypass.
Information for you
Bariatric and metabolic surgery
Bipartition of intestinal transit
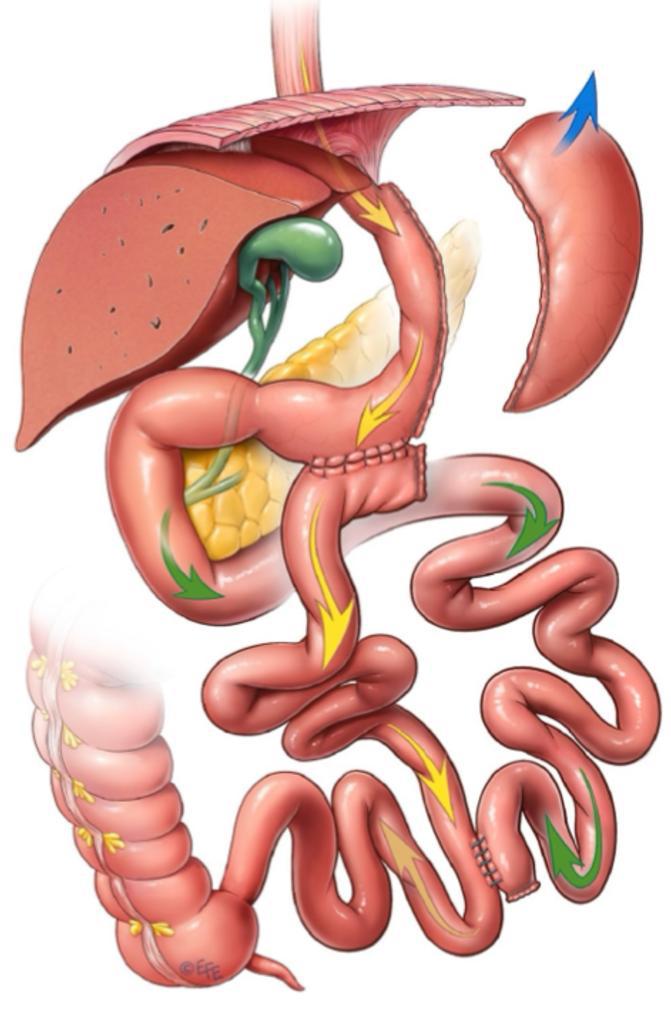
BTI is a metabolic-bariatric surgery technique that involves creating two pathways for food to bypass a portion of the small intestine. Bipartitioned intestinal transit is a surgical technique that has revolutionized the approach to obesity and type 2 diabetes. It consists of reconfiguring the small intestine, dividing it into two segments. This anatomical modification induces physiological changes that promote weight loss and glycemic control.
Physiological bases:
- Increased secretion of incretins: Incretins are intestinal hormones that stimulate the release of insulin and reduce the production of glucagon, which improves glycemic control (current medications for diabetes and weight loss arose as a result of this type of ileal surgeries (due to their anatomical confirmation towards the terminal ileum).
- Increased exposure of the intestinal epithelium to bile acids: This modification alters the absorption of fats and promotes the feeling of satiety.
- Modification of the intestinal microbiota: The new intestinal configuration influences the composition of intestinal bacteria, which can contribute to weight loss and improved metabolism.
Advantages over other procedures:
- Greater simplicity: It is a less complex technique than other bariatric surgeries, which translates into shorter surgical times and a lower risk of complications.
- Better metabolic results: Studies have shown that bipartitioned intestinal transit is highly effective in the remission of type 2 diabetes and sustained weight loss.
- Lower risk of malabsorption: Unlike other techniques that can cause severe nutritional deficiencies, intestinal transit bipartition usually preserves the absorption of essential nutrients.
Bipartition of intestinal transit is a promising surgical option for the treatment of obesity and type 2 diabetes. Its mechanism of action is based on physiological modifications that promote weight loss and glycemic control. The simplicity of the technique, together with its excellent results, position it as an attractive alternative to other bariatric procedures. Schedule your appointment to learn more details.
Projets de voyage
Learn how to schedule and plan your surgery
We offer excellent accommodation and travel plans so that you do not have to worry about anything when it comes to your surgeries or treatments.